Movement impairment has been thought to live within a perpetual cycle, feeding deeper dysfunction and pain through the passage of time. Such a cycle is known as the chronic musculoskeletal pain cycle (CMPC) (Page, Lardner, & Frank, 2010). Knowledge of the aforementioned phenomenon demands vigilance and a proactive sensibility from the exercise professional when training clientele, and developing programs. However, a process must first exist to screen out subtle, and sometimes insidious, movement dysfunctions before mitigating the CMPC. Thus, the following will examine such a screening process, known as the functional movement screen (FMS), in addition to outlining its key concepts, efficaciousness, and clinical utilities.
Movement impairment has been thought to live within a perpetual cycle, feeding deeper dysfunction and pain through the passage of time. Such a cycle is known as the chronic musculoskeletal pain cycle (CMPC) (Page, Lardner, & Frank, 2010). Knowledge of the aforementioned phenomenon demands vigilance and a proactive sensibility from the exercise professional when training clientele, and developing programs. However, a process must first exist to screen out subtle, and sometimes insidious, movement dysfunctions before mitigating the CMPC. Thus, the following will examine such a screening process, known as the functional movement screen (FMS), in addition to outlining its key concepts, efficaciousness, and clinical utilities.
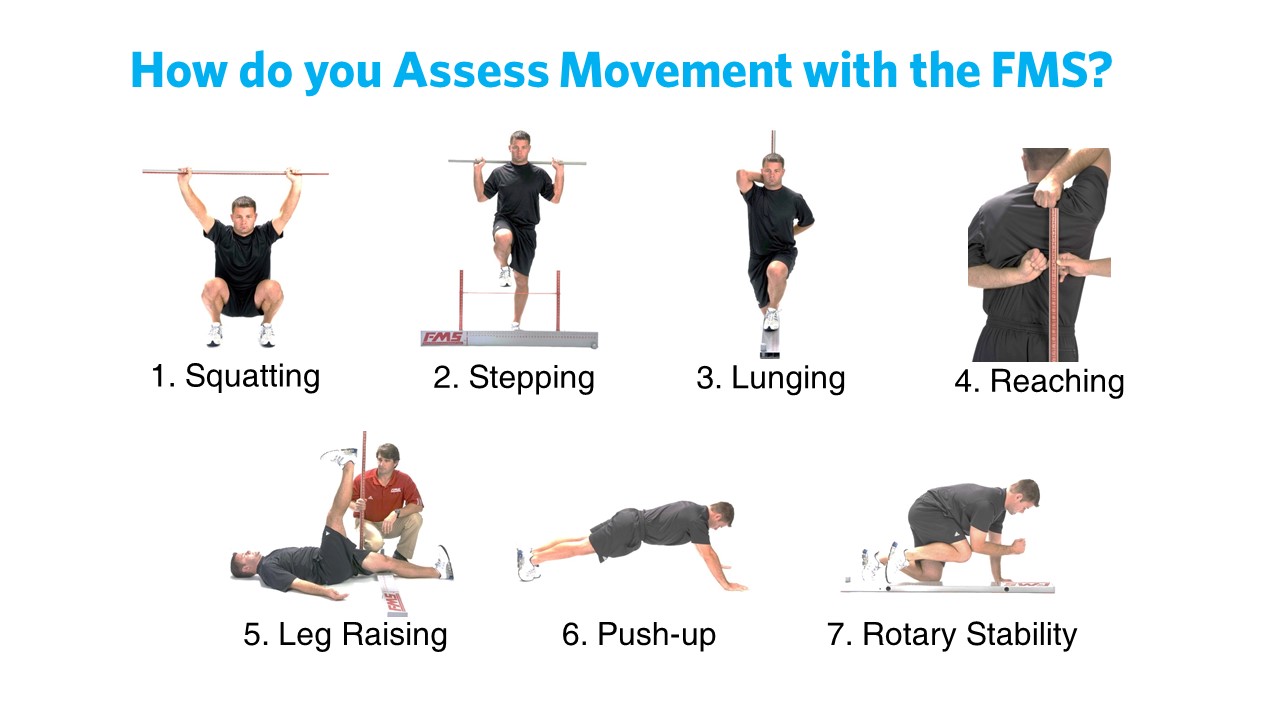
The FMS is an aggregate of 7 screens consisting of the: active straight leg raise (ASLR), shoulder mobility (SM), rotary stability (RS), trunk stability push-up (TPSU), in-line lunge (ILL), hurdle step (HS), and deep squat (DS) (Cook, Burton, Hoogenboom, & Voight, 2014). Additionally, the 7 movement screens are supplemented with 3 clearing tests to detect pain: the shoulder impingement test, spinal extension test, and spinal flexion test (Cook et al., 2014). Specific pain tests were included as Cook et al. (2014) noted that the 7 movement screens might not be sensitive enough to uncover painful motions. Thus, the additional pain tests were included as a proactive measure, graded as positive if there is pain, and negative if there is no pain (Cook et al., 2014).
Each movement screen contains within it, a 4-level grading system as a means of quantifying the quality of each movement pattern. These include 0, 1, 2, and 3 (Cook et al., 2014). 0 is indicative of pain reported during the test; Cook et al. (2014) noted that a movement screen would receive a grade of 0 if there were pain, regardless of whether the movement pattern quality received a grade of 1, 2, or 3. Cook et al. (2014) took such a position as a means of avoiding exercises that could worsen the pattern/pain, and to provide an opportunity to refer the client to a medical professional that could properly address the functional pathology. A grading of 1 indicates the movement was not completed or performed adequately. A grading of 2 indicates completion of the movement with some compensatory motions, and a grading of 3 indicates completion of the movement without the presence of compensations (Cook et al., 2014).
The 7 movement screens from the FMS are predicated on several concepts borrowed from other researchers and medical practitioners, such as Vladimir Janda. Janda began challenging traditional structural approaches to dysfunction and pain in the mid 1900s, which focused exclusively on the site of discomfort (Page et al., 2010). During this time, Janda submitted that a different paradigm was necessary to fully comprehend the nature of pain; he suggested embracing a functional approach, whose purpose was to uncover the source and cause of pain through observation of the sensorimotor system, motion, and basic movement patterns (Page et al., 2010). Similar to Janda’s approach, the FMS recognized dysfunctional movement patterns as a representation and consequence of poor motor control and muscle imbalances, considered the progenitors of pain (Cook et al., 2014). Ultimately the authors’ goals were to create a screening process that would: identify individuals at risk of injury, assist in developing corrective exercise to fix impaired movement patterns, provide a tool to systematically track progress and change, and to create a functional baseline that would allow a rating system of dysfunctional movement patterns (Cook et al., 2014).
The FMS and the associated tests within it, consider movement quality (i.e., smooth and coordinated movement) over performance output (i.e., maximum force production, power, cardiac output etc…) as the foundations to program design and injury prevention (Cook et al., 2014). Similar to Janda’s movement assessments, the FMS attempts to capture the coordination of prime movers, synergists, and stabilizers, considered the foundations of motion (Page et al., 2010). Focus is placed on the smooth sequencing and coordination of movement, instead of isolated muscle and joint performance, because the latter does not provide requisite insight into robust, multi-joint and multi-muscle motions, considered the method in which the body truly operates (Cook et al., 2014). In essence, both approaches of Janda and the FMS recognize and abide by the motor learning concept of coordinative structures; the body coordinates many muscles simultaneously in the form of patterns, instead of controlling each muscle and joint individually (Magill, 2011).
Having considered the intents and philosophical underpinnings of the screen, the FMS is not impervious to questions of validity. Validity can be defined as the degree to which a test is intended to measure what it is supposed to measure (Beardsley & Contreras, 2014). When reviewing the validity of the FMS tests, face validity (FV) is of particular interest. FV is defined as the degree to which a test is perceived by the subject to measure what it is intended to measure (Beardsley & Contreras, 2014). A repeated measures experiment by Frost, Beach, Callaghan, and McGill (n.d.) using 21 firefighter subjects questioned such validity of the FMS. Frost et al. (n.d.) performed two approaches of implementing the FMS in which one method included only explaining what to do (i.e., providing verbal instructions). The second method included verbal instructions in addition to explaining the purpose of each screen (i.e., what each screen is looking for in terms of dysfunction, and grading criteria). When comparing both approaches, performance outcomes improved significantly in the experiment which included verbal instruction and grading criteria, when compared to verbal instruction only (Frost et al., n.d.).
In conclusion, the FMS is not without criticism. However, it does strive to implement best practice with contemporary concepts such as regional interdependence, motor control theory, and CMPC (Cook et al., 2014). Additionally, the FMS is replete with simplicity of use, educational support, and infrastructure. Thus, the movement screens could be implemented as part of a larger group of skill sets, which the exercise professional could access and draw from, when interacting with clientele.
References
Beardsley, C., & Contreras, B. (2014). The Functional Movement Screen: A review. Strength and Conditioning Journal, 36(5), 72-80.
Cook, G., Burton, L., Hoogenboom, B.J., & Voight, M. (2014). Functional movement screening: The use of fundamental movements as an assessment of function – Part 1. The International Journal of Sports Physical Therapy, 9(3), 396-409.
Cook, G., Burton, L., Hoogenboom, B.J., & Voight, M. (2014). Functional movement screening: The use of fundamental movements as an assessment of function – Part 2. The International Journal of Sports Physical Therapy, 9(4), 549-563.
Frost, D.M., Beach, T.A.C., Callaghan, J.P., & McGill, S.M. (in press). FMS scores change with performers’ knowledge of the grading criteria – Are general whole-body movement screens capturing “dysfunction”? Journal of Strength and Conditioning Research.
Magill, R. A. (2011). Motor learning and control: Concepts and applications (9th ed.). New York: McGraw-Hill.
Page, P., Lardner, R., & Frank, C. (2010). Assessment and treatment of muscle imbalances: The Janda approach. Champaign, IL: Human Kinetics.
-Michael McIsaac