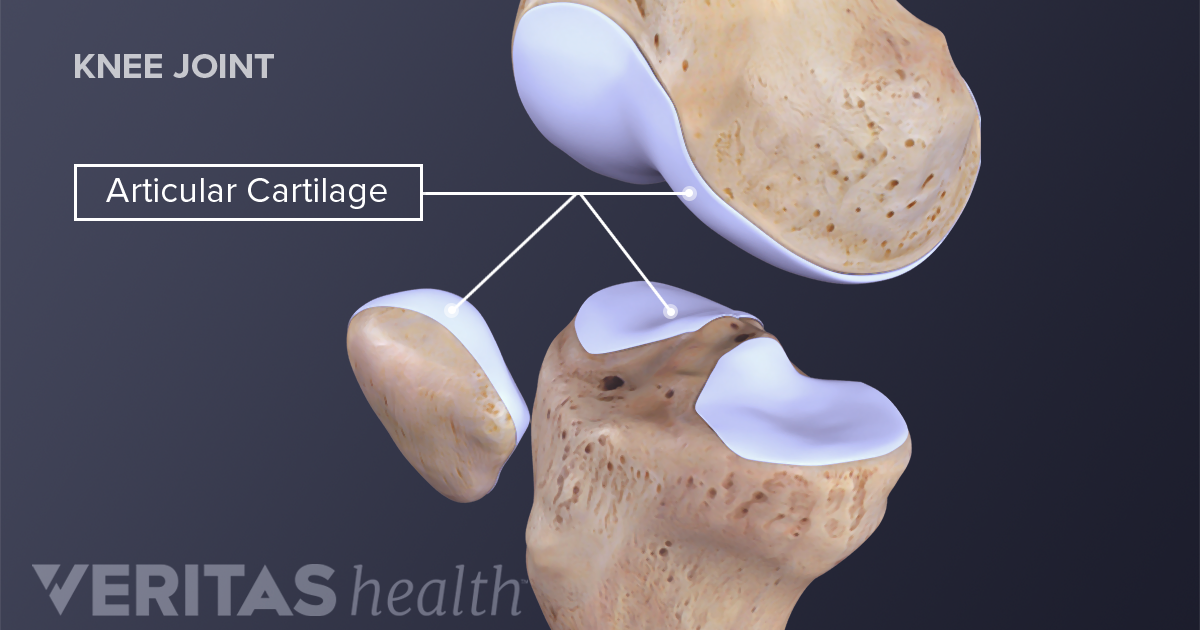
Osteoarthritis (OA) is a common disabling condition characterized by degenerative changes in articular cartilage and underlying bone.1 Degeneration ensues when the balance of cartilage synthesis and breakdown becomes disrupted. Left unmitigated, deeper deterioration of articulating surfaces emerges causing pain, decreased mobility, and lowered quality of life. Therefore, it is imperative to consider interventions which help manage degenerative changes in an attempt to protect and regain pain-free mobility. As such, the following will consider type 2 collagen (T2C) as a potential means of controlling osteoarthritic pain and mobility restrictions.
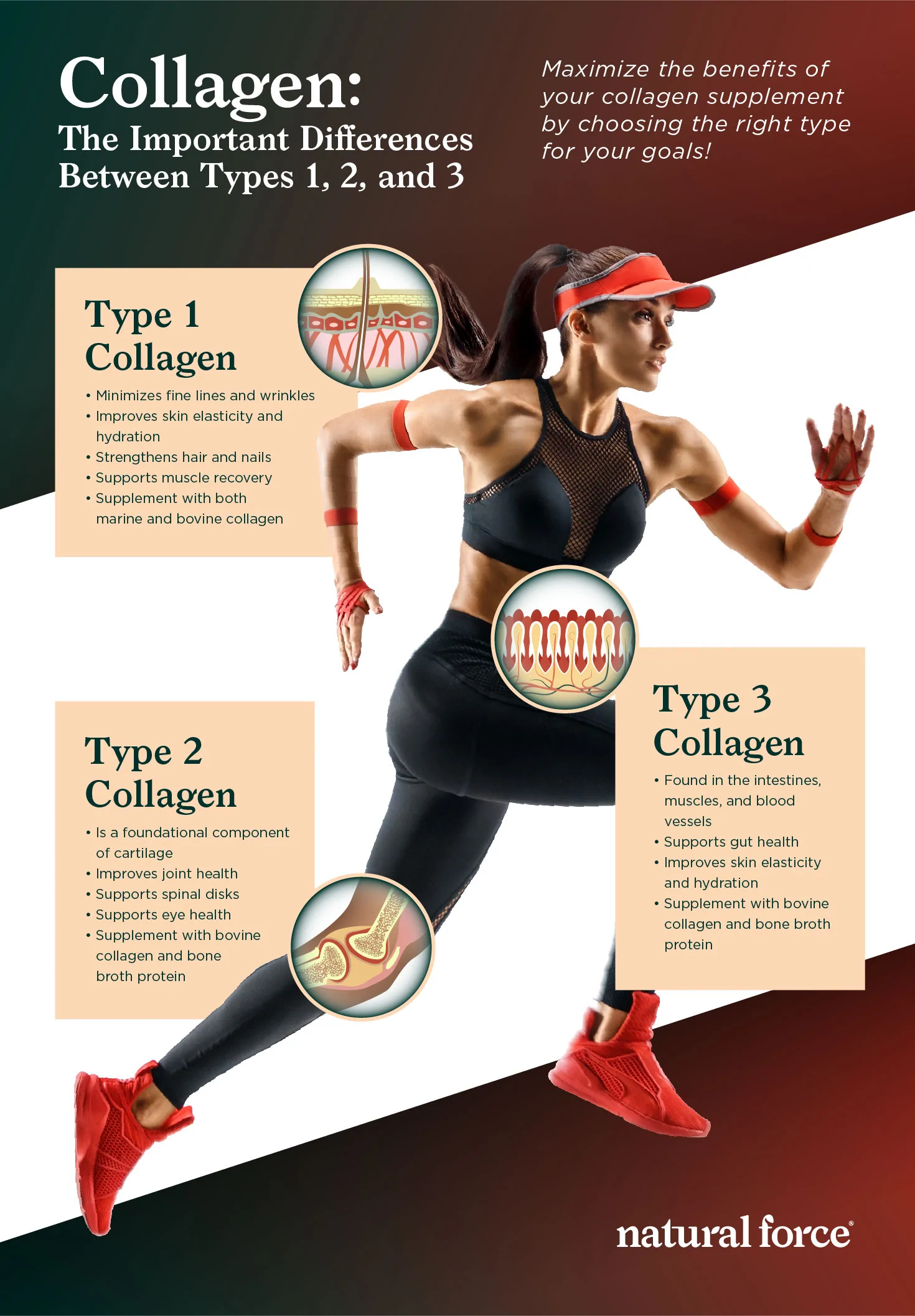
Cartilage is the substance which lines the surfaces of joints and allows for smooth and pain-free articulation. The main component of cartilage is a substance known as T2C.1(96) When degeneration of cartilage is present, the kidneys release associated degradation products in the urine, which can be measured and correlated with the degree of damage present. Interestingly, oral T2C (derived from chicken sternum) down-regulates T-Cells (a type of white blood cell responsible for destroying other cells) which are known to attack structural T2C in the cartilage.1(96) Such suggests that T2C might have immunomodulating effects upon OA.
Ultimately, oral T2C is thought to keep the immune system from recognizing and attacking endogenous (within the body) T2C which helps minimize cartilage degeneration. Such can be tracked by a reduction in lowered C-terminal telopeptide; a component of T2C, which can be found in the urine.1(96) Having briefly considered both immunological and histological events as they relate to OA and T2C, the following will explore the efficacy of T2C in controlling joint pain and function.
Bakilan et al.1(96) constructed a study whereby subjects between the ages of 45-70 who had been diagnosed knee OA were recruited to explore the effects of oral T2C, as an adjunct intervention, upon managing joint pain and function. Subjects were excluded if they underwent processes to manage OA such as physiotherapy, intraarticular injections, knee surgery, oral treatments (i.e., glucosamine) among others. After such exclusion criteria was considered, 39 subjects were available for said study.1(96)
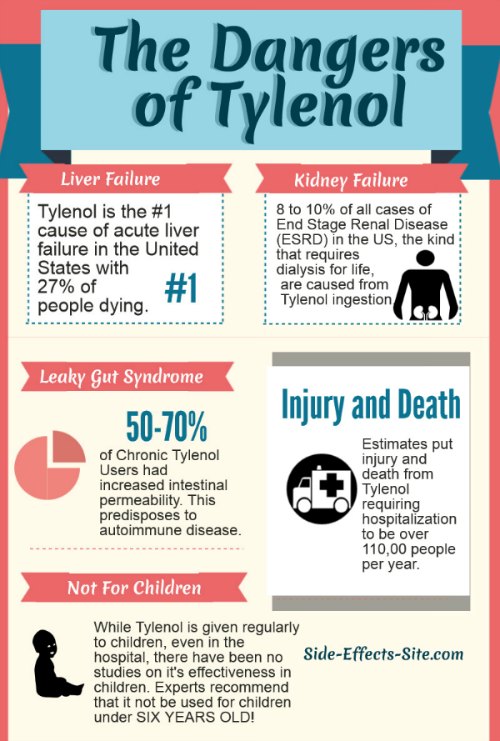
The study was a randomized, single blind and controlled clinical study which took place over a 12-week period. 19 subjects were randomly assigned to a group who would receive acetaminophen (AC group) at 1500 mg/day, while 20 other subjects were assigned to a group that would receive 1500 mg/day of AC + 10 mg T2C (AC+T2C group).1(96) One primary outcome measure for both groups included pain at rest and during walking, assessed from 0 (no pain) to 10 (worst possible pain) on a Visual Analogue Scale Score (VAS). Said measure was completed before, and after, the intervention.
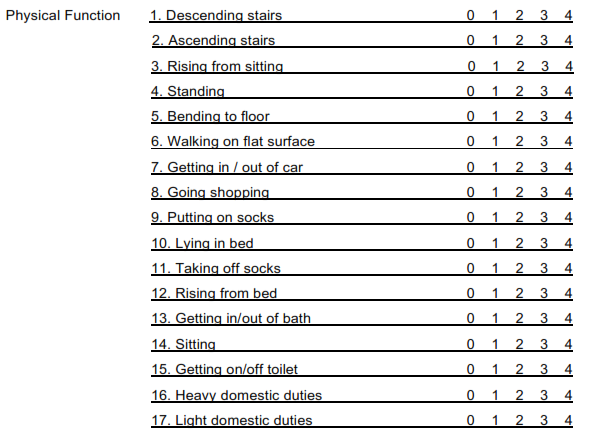
The second primary outcome measure was intended to assess function/mobility via the Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) and 20 metre walking time and short form-36 (SF-36).1(96) WOMAC is a widely used set of standardized questionnaires to evaluate and track individuals with osteoarthritis of the hip and knee, including stiffness, pain, and physical functioning of the aforementioned joints.1(96) SF-36 calculates 8 multi-item scales to include general health, bodily pain, social role functioning, mental health, vitality, emotional role, physical role, physical functioning.1(97) Said measures were completed before, and after, the intervention.
Interestingly, after the 12-week intervention, the AC+T2C group reported significant improvements in pain, function, and quality of life compared to baseline; the AC group only reported improvements in quality of life with no improvements in pain or function when compared to baseline.1(97) Considering that popular treatment of OA typically includes only AC and NSAIDs (which do have side effects) with physical therapy/exercise/heat and cold therapy, the addition of T2C as a safe and effective adjunct appears promising.2
Though the above study explored AC and T2C therapy, it should be noted that such an approach need not live in a vacuum; the below articles written previously by this author have provided other supportive interventions, which help manage arthritic symptoms. It is likely that combining multiple approaches would have an aggregating effect upon AR. Ultimately, the research by Bakilan et al.1(97) has suggested that T2C is a candidate for therapy in managing the debilitating effects of OA, and a likely adjunct intervention with other approaches as outlined below.
Please see below links exploring other interventions to manage osteoarthritis:
Osteoarthritis and Nutritional Support
Osteoarthritis and Omega-3 Fatty Acids
Osteoarthritis and Platelet-Rich Plasma
Osteoarthritis, Inflammation, and Saunas
Bromelain and Osteoarthritis
Osteoarthritis and Yucca Schidigera
References
1. Bakilan F, Armagan O, Ozgen M, et al. Effects of native type II collagen treatment on knee osteoarthritis: A randomized controlled trial. Eurasian J Med. 2016;48:95-101. doi: 10.5152/eurasianjmed.2015.15030.
2. Crowley DC, Lau FC, Sharma P, et al. Safety and efficacy of undenatured type II collagen in the treatment of osteoarthritis of the knee: a clinical trial. Int J Med Sci. 2009;6(6):312-321. doi: 10.7150/ijms.6.312.
-Michael McIsaac