In my last post, anthropometric assessments (body mass index, waist circumference, skinfold measurements, and bioelectrical impedance) were considered as a means of exploring an individual’s nutritional and health status. Although such measures are considered useful, biochemical tests provide another layer of screening designed to provide deeper objective and quantitative findings. Such biomarkers, in conjunction with body measurements and standard food questionnaires, can allow a nutritionist to provide more guided and efficacious nutritional interventions. As a means of appreciating the utility of such biochemical measures, the following will consider two tests that determines protein status within an individual: the creatinine height index (CHI) test and nitrogen balance test.
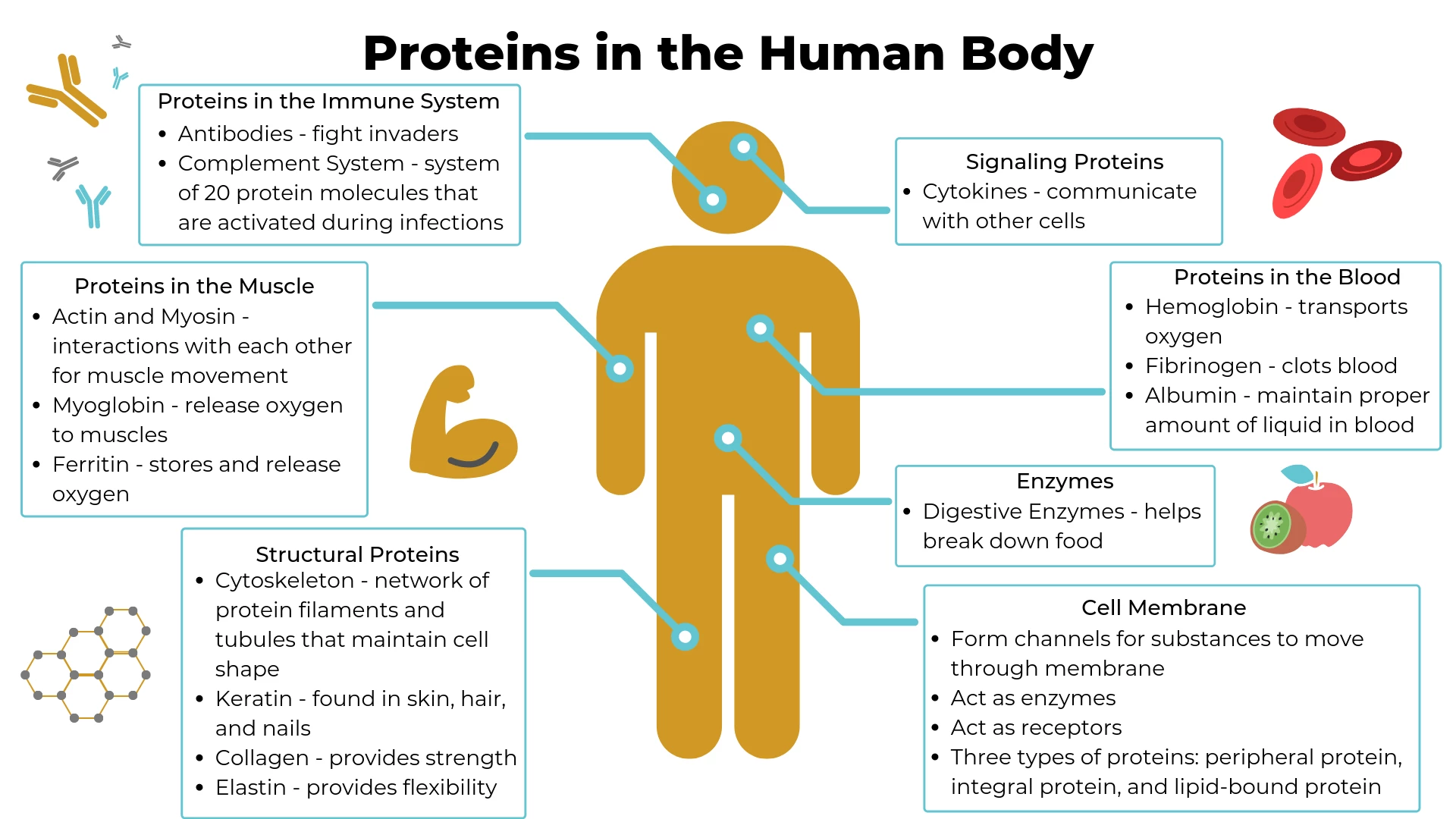
Lee and Nieman (2013) indicated that protein can be assessed by way of somatic and visceral analysis. Somatic protein represents 75% of body cell mass (metabolically available protein) and is found within skeletal muscle, while visceral protein comprises 25% of body cell mass and is found within the organs of the body (i.e., kidneys, heart), erythrocytes (i.e., red blood cells), and granulocytes/lymphocytes (i.e., white blood cells) (Lee and Nieman, 2013). As an aggregate, somatic and visceral protein constitutes 30%-50% of total body protein. Thus, deficiencies in such a macronutrient can have a deleterious effect on the protein pool and availability.
Protein deficiency can induce protein-energy malnutrition (PEM), characterized by the progressive loss of both lean body mass and adipose tissue resulting from primary (insufficient consumption of protein and energy) and secondary (malabsorption or increased requirement of protein) conditions (Hengeveld et al., 2018). Lee and Nieman (2013) stated that although PEM is not considered a wide-sweeping deficiency in developed nations, the condition can still occur in those afflicted with cancer, the homeless, individuals with acquired immune deficiency syndrome, and children who fail to thrive. Thus, implementation of a protein status tests is still relevant in developed nations with such conditions. The following will briefly explore frequently used protein status tests to appreciate their utility in the prevention and diagnosis of PEM.
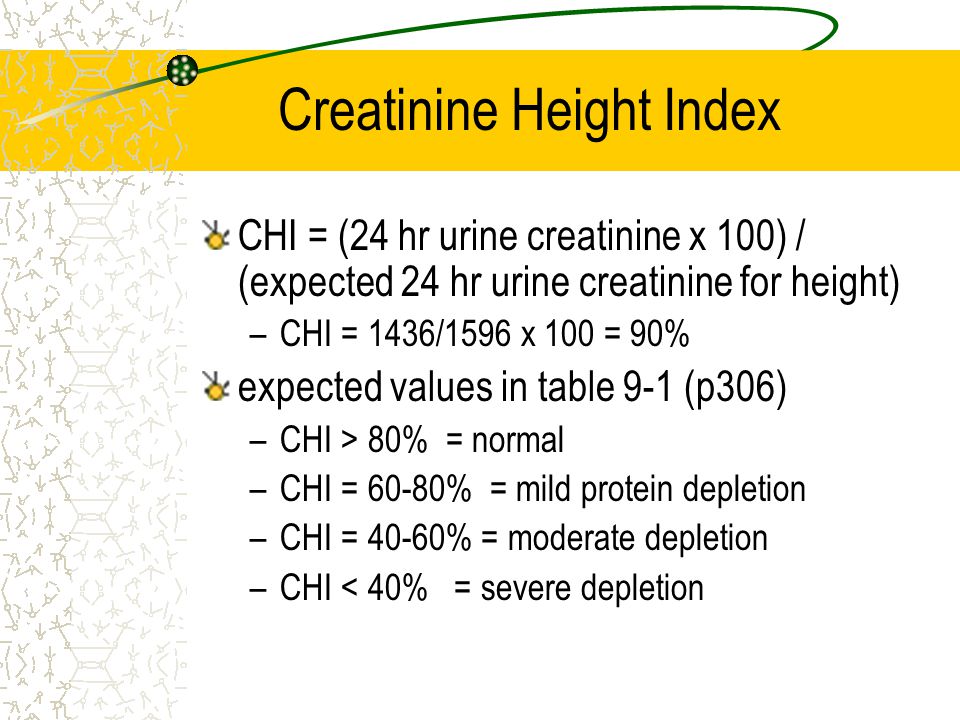
CHI = (24 hr urine creatinine x 100) / (expected 24 hr urine creatinine for height) CHI = 1436/1596 x 100 = 90% expected values in table 9-1 (p306) CHI > 80% = normal. CHI = 60-80% = mild protein depletion. CHI = 40-60% = moderate depletion. CHI < 40% = severe depletion.
The creatinine height index test (CHI) is considered a sensitive indicator of nutritional status and lean body mass (somatic) in adults (Datta, Wu, Grady, & Scalise, 2018).Creatinine is a protein stored in the skeletal muscle, which is metabolized and dispersed at a constant rate. As such, the 24-hour urine creatinine excretion provides an approximation of muscle mass (Datta et al., 2018).CHI is defined as the 24-hour urine creatinine of a patient divided by the expected 24-hour creatinine of a normal adult of the same sex and height (Lee and Nieman, 2013). Furthermore, CHI is expressed as a percent of expected value; a CHI of 60%-80% indicates mild protein depletion, 40%-60% represents moderate protein depletion, while values below 40% indicate severe depletion (Lee and Nieman, 2013). Although CHI is considered a sensitive indicator of somatic protein status, the test can still be limited by an individual’s diet, variability in creatinine excretion, and the use of height-weight tables for determining expected creatinine excretion (Lee and Nieman, 2013).
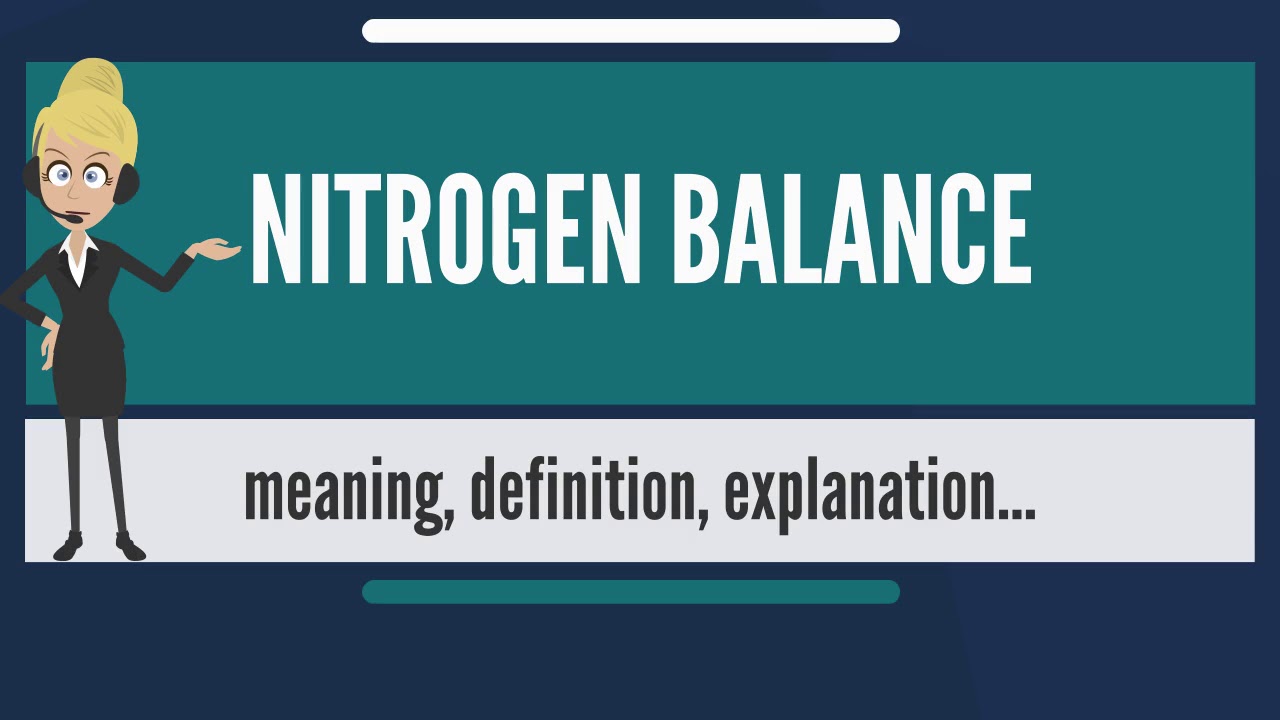
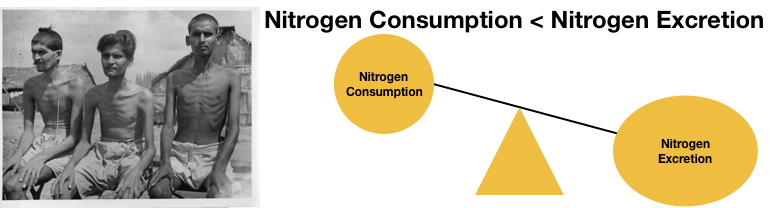
Nitrogen balance is a second method in determining protein status within an individual. Nitrogen, consumed as protein in the diet, has a relationship to nitrogen lost through the urine; positive nitrogen balance is defined as protein intake (consumption) that exceeds protein degradation (nitrogen loss through urine) also known as an anabolic (building of molecules) state. Positive nitrogen balance is often seen in those who are in childhood (growing) or individuals recovering from trauma, recovery, or illness (Lee and Nieman, 2013). Conversely, negative nitrogen balance is characterized by protein intake that is below protein degradation causing a catabolic (breakdown of molecules) state. Such a deficit in nitrogen is seen in those who have experienced sepsis, surgery, cancer, extended bed rest, and gastrointestinal disease (Lee and Nieman, 2013).
Nitrogen balance is determined by a 24-hour measurement of protein intake (g/24hr) in conjunction with an estimate of nitrogen losses from the body. Nitrogen intake is estimated by dividing total protein intake by 6.25, while nitrogen loss is calculated by measuring urine nitrogen levels and adding a constant (helps account for nitrogen lost in skin, stool, wound drainage, nonurea nitrogen) (Lee and Nieman, 2013). Although considered a useful measure in the general population, such a test is limited within individuals experiencing burns, vomiting, diarrhea, and fistula drainage (harder to measure and estimate nitrogen lost through said conditions) (Lee and Nieman, 2013).
In conclusion, gathering urine samples to measure creatinine or nitrogen levels provides a relatively non-invasive means of determining protein status, and ultimately the health, of individuals. However, said tests also has within them, limitations that must be considered and weighed when assessing a client. However, when paired with other measures of health status (i.e., waist circumference, BMI, bioelectrical impedance, skinfold measures, nutritional questionnaires), the aggregation of data might help offset the inherent limitations of each biomarker. Ultimately, such an approach should help lead the nutritionist towards more meaningful and effective interventions.
References
Datta, D., Foley, R., Wu, R., Grady, J., Scalise, P. (2018). Can creatinine height index predict weaning and survival outcomes in patients on prolonged mechanical ventilation after critical illness? Journal of Intensive Care Medicine, 33(2), 104-110.
Hengeveld, L. M., Wijinhoven, H. A. H., Olthof, M., Brouwer, I. A., Harris, T. B., Kritchevsky, S. B., … Visser, M. (2018). Prospective associations of poor diet quality with long-term incidence of protein-energy malnutrition in community-dwelling older adults: The health, aging, and body composition (Health ABC) study. The American Journal of Clinical Nutrition, 107(2), 155-164.
Lee, R. D., & Nieman, D. C. (2013). Nutritional assessment (6thed.). New York, NY: McGraw-Hill.
-Michael McIsaac