GENERAL OVERVIEW
Thyroidectomy is a procedure whereby part, or all, of the thyroid gland is removed.1 Such a surgery is conducted to address and treat thyroid disorders to include: overactive thyroid (hyperthyroidism), thyroid gland enlargement (goiter), and thyroid cancer.1 If partial thyroid gland removal is undertaken, the remaining glandular tissue is likely to continue producing thyroid hormone (i.e., T3 and T4). If a thyroid gland is removed in its entirety, the patient will require thyroid hormone replacement.1 To learn more about thyroid function, thyroid conditions, and interventions related to the same, please see the links below.
Thyroid Hormone Regulation and Health
Hashimoto’s Thyroiditis and Nutritional Support Hashimoto’s Thyroiditis: Connection to Gut Function, and Solutions
Environmental Toxins and Thyroid Function
Iodide Function and Sources
Selenium: Function, Deficiencies, and Best Sources
COMPLICATIONS
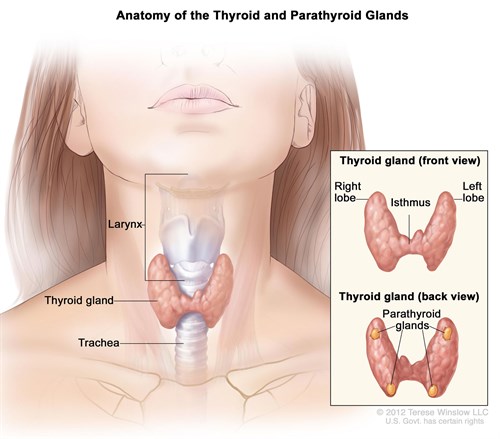
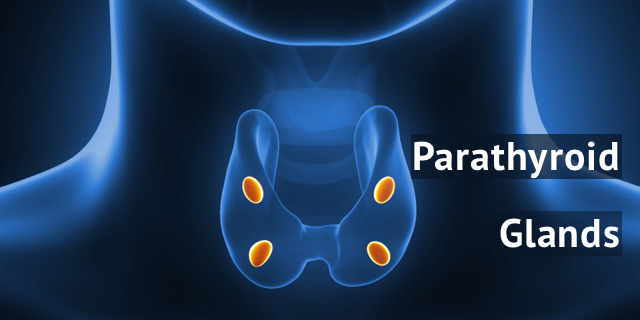
Thyroidectomies are not completely devoid of risks; occasionally, the parathyroid (resting behind the thyroid gland) can become negatively affected; such can occur from thyroid carcinoma, experience of the surgeon, iatrogenic (inadvertent) surgical trauma, extent of the surgery, degree of undamaged parathyroid tissue remaining, and retrosternal goiter.2 Ultimately, the parathyroid can become compromised during thyroidectomies.
PARATHYROID IN GREATER DETAIL
The parathyroid gland’s primary function is to synthesize and release parathyroid hormone (PTH); a substance responsible for regulating serum calcium concentrations.4 PTH inhibits osteoblast (development of bone) activity and stimulates osteoclast (breakdown of bone/release of calcium).4 PTH also stimulates the kidneys to resorb calcium (i.e., reduce loss of calcium) and produce biologically active vitamin D; vitamin D facilitates absorption of calcium from food in the small intestine, among a myriad of other roles.4
Interestingly, PTH and calcium levels have an inverse relationship; when calcium is low, PTH (and vitamin D) stimulate multiple sites to mobilize stored calcium. When calcium levels reach normal levels in the blood, PTH and vitamin D provide feedback to the parathyroid to decrease PTH.4
PARATHYROID DAMAGE / REDUCED PTH
If the parathyroid is damaged/removed during a thyroidectomy, calcium levels can become dysregulated. Such an event can induce a condition known as hypoparathyroidism-related hypocalcemia.5 Transient hypocalcemia was reported to occur in 16-55% of total thyroidectomy cases, while another study indicated that patients who developed post-operative hypocalcemia also had hypoparathyroidism for over 4 weeks after surgery.6 Shafer and Shoback6 also noted that 35% of patients with total thyroidectomies (retrospective study) experienced hypocalcemia for 6 months; 1.4% of patients experienced hypoparathyroidism for 2 years after total thyroidectomies.
MORE ON HYPOCALCEMIA
It is standard general practice to closely monitor calcium levels after thyroidectomies for reasons noted above. Shafer and Shoback6 stated that analyzing serum calcium levels over 16 hours post-operatively was adequate to screen patients for risk of hypocalcemia. Symptoms from said condition can include neuromuscular irritability (hallmark presentation), neurological issues, cognitive problems, skin related issues, smooth muscle challenges, ophthalmologic manifestations, and cardiac events.6
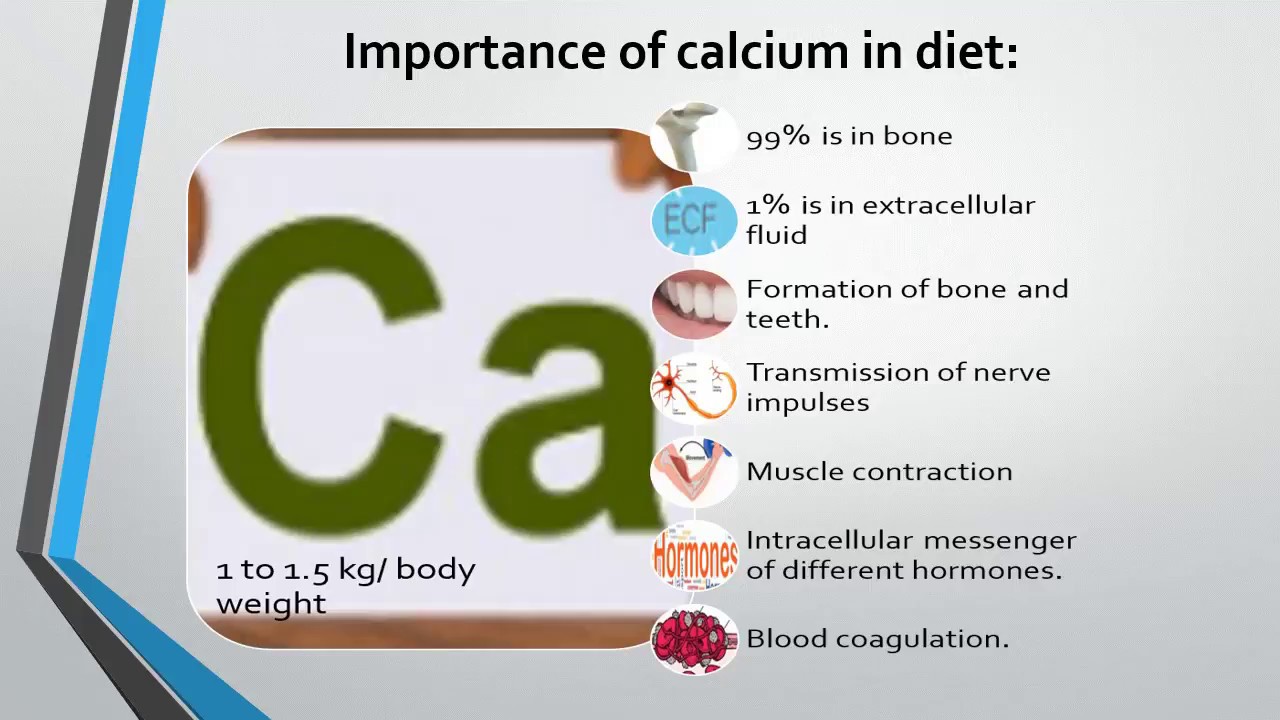
ROLES OF CALCIUM
Calcium is critical for development of bones/bone density, muscle contraction, nerve impulses, blood clotting, signal transmission, fluid balance, and regulation of heartbeats.8 Daily requirements (individuals without parathyroid issues) of calcium fall within the range of 450 mg.8(660)
TREATING HYPOCALCEMIA
If an individual experiences a precipitous drop in serum calcium levels, such a condition can be life-threatening and requires immediate medical intervention.6 Generally, calcium gluconate is used via intravenous means to treat said condition. However, if a patient has chronic hypocalcemia (perhaps from partial parathyroid loss) other means of treatment are available.
Interestingly, chronic hypocalcemia (even towards severe hypocalcemia) can remain asymptomatic.6 If chronic hypocalcemia exists beyond hospital stay/surgery, oral calcium carbonate (40% elemental calcium) can be administered in 1-3 grams split over 3-4 divided doses with foods (optimized absorption).6 Said calcium levels can be measured every 3-6 months to ensure levels remain in optimal ranges.6 If hypoparathyroidism remains, supplemental vitamin D3 may also be indicated to facilitate calcium absorption from food/supplements.7
CONCLUSIONS
Thyroidectomies are procedures in which part, or all, of the thyroid gland is removed. Such a surgery is conducted to address and treat thyroid disorders to include: overactive thyroid (hyperthyroidism), thyroid gland enlargement (goiter), and thyroid cancer. However, during said procedures, the parathyroid gland can become damaged (iatrogenic) or removed by necessity. Such can induce aggressive hypocalcemia which must be summarily addressed. However, chronic hypocalcemia can also occur, which may require longer term use of calcium/vitamin D supplementation. Such approaches should not only help individuals recover from thyroidectomy surgeries; close monitoring of calcium levels/intake also provides an opportunity to support general health, performance, and longevity.
Reference
1. Thyroidectomy. Mayo Clinic. Updated September 3, 2022. Accessed September 8, 2022. https://www.mayoclinic.org/tests-procedures/thyroidectomy/about/pac-20385195.
2. Tolone S, Roberto R, Genio G, et al. The impact of age and oral calcium and vitamin D supplements on postoperative hypocalcemia after total thyroidectomy. A prospective study. BMC Surg. 2013;13(Suppl 2):1-6. doi:10.1186/1471-2482-13-S2-S11.
3. Khan M, Jose A, Sharma S. Physiology, parathyroid hormone. StatPearls. Treasure Island, FL: StatPearls Publishing; 2022. https://www.ncbi.nlm.nih.gov/books/NBK499940/. Updated June 28, 2022. Accessed September 8, 2022.
4. Lofrese JJ, Basit H, Lappin SL. Physiology, parathyroid hormone. StatPearls. Treasure Island, FL: StatPearls Publishing; 2022. https://www.ncbi.nlm.nih.gov/books/NBK482510/. Updated July 18, 2022. Accessed September 16, 2022.
5. Tramontano S, Sarno G, Calabrese P, et al. Does time matter in deficit of calcium after total thyroidectomy in subjects with previous bariatric surgery? Nutrients. 2022;14(1805):1-8. doi: https://doi.org/10.3390/nu14091805.
6. Schafer AL, Shoback DM. Hypocalcemia: Diagnosis and treatment. Endotext. South Dartmouth MA. MDText Inc; 2000. https://www.ncbi.nlm.nih.gov/books/NBK279022/. Updated January 3, 2016. Accessed September 16, 2022.
7. Khazai N, Judd SE, Tangpricha V. Calcium and vitamin D: Skeletal and extraskeletal health. Curr Rheumatol Rep. 2009;10(2):110-117. doi:10.1007/s11926-008-0020-y.
8. Pravina P, Sayaji D, Avinash M. Calcium and its role in the body. Int J Res Pharm Biomed Sci. 2013;4(2):659-668. doi: https://www.researchgate.net/publication/274708965.
-Michael McIsaac