In my last article, risk factors for COVID-19 disease virulence, and micronutrient recommendations to support the immune system, were explored. One of the major risk factors for disease severity, previously outlined, included metabolic syndrome (MS); a constellation of risk factors, that when combined, increase an individual’s chances of contracting conditions such as heart disease, stroke, and diabetes.1 Evidence has suggested that individuals who harbour MS have significantly increased risk of severe COVID-19 symptoms. As such, the following will consider the pathophysiological aspects of MS thought to increase virulence, as well as solutions to mitigate MS.
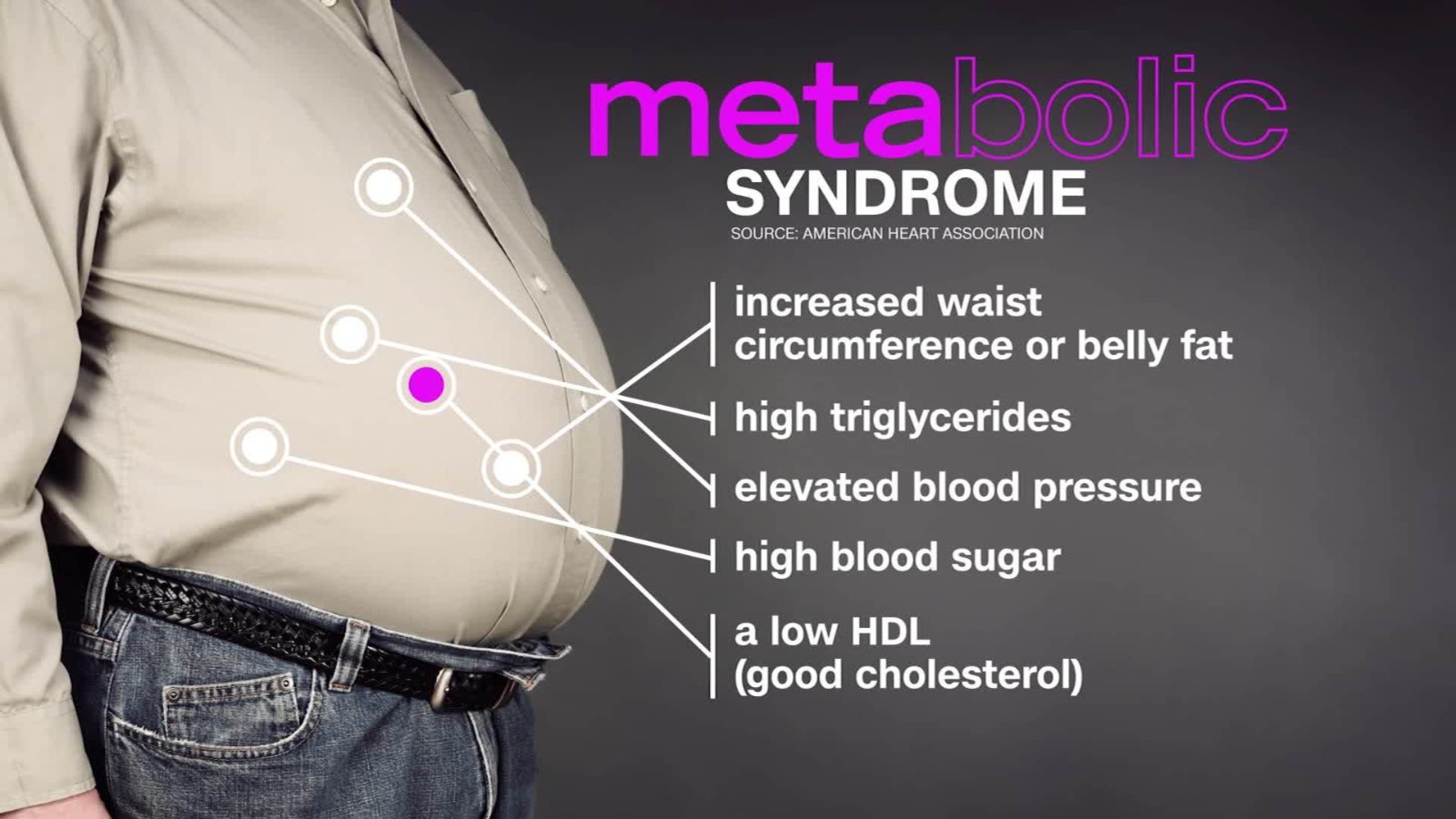
As mentioned, MS is characterized by the prevalence of heart disease, stroke, and diabetes. However, MS can also be characterized by the underlying drivers/risk factors of said clinical conditions. Such would include high triglyceride levels, increased waistline/adiposity, low high-density lipoproteins, high levels of blood sugar/insulin resistance, high blood pressure, and low-grade chronic inflammation.3 Such drivers of MS have implications on COVID-19 disease progression.
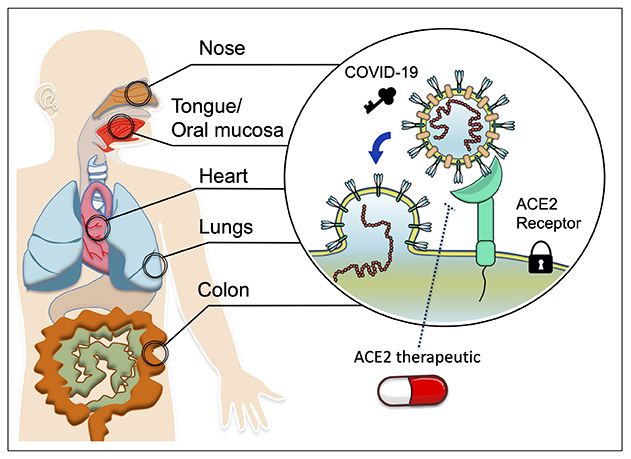
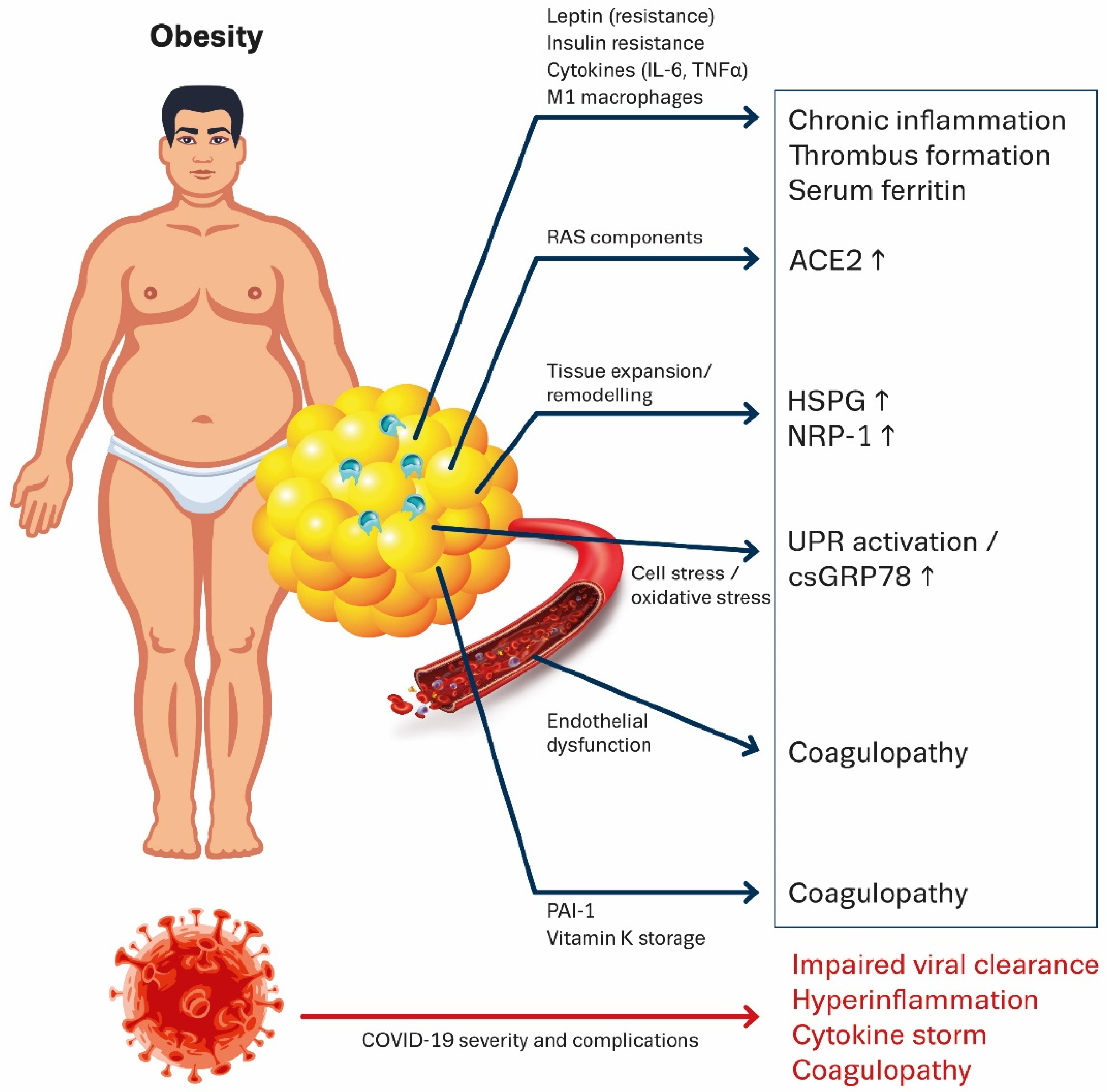
SARS-CoV-2 has a strong affinity towards ACE-2 receptors; the gateway for viral entry, replication, and tissue damage. ACE-2 is highly expressed (aka abundant) in myocardial cells, kidney cells, bladder/urethra cells, small intestine cells, nervous system cells, and lung cells.4 However, increased fatty tissue found in obesity (a risk factor for MS) has a significantly higher expression of ACE-2 receptors compared to individuals with low levels of adiposity.2(361) Such may provide greater opportunities (or doorways) for the virus to enter, replicate, and damage organ systems.2(361)
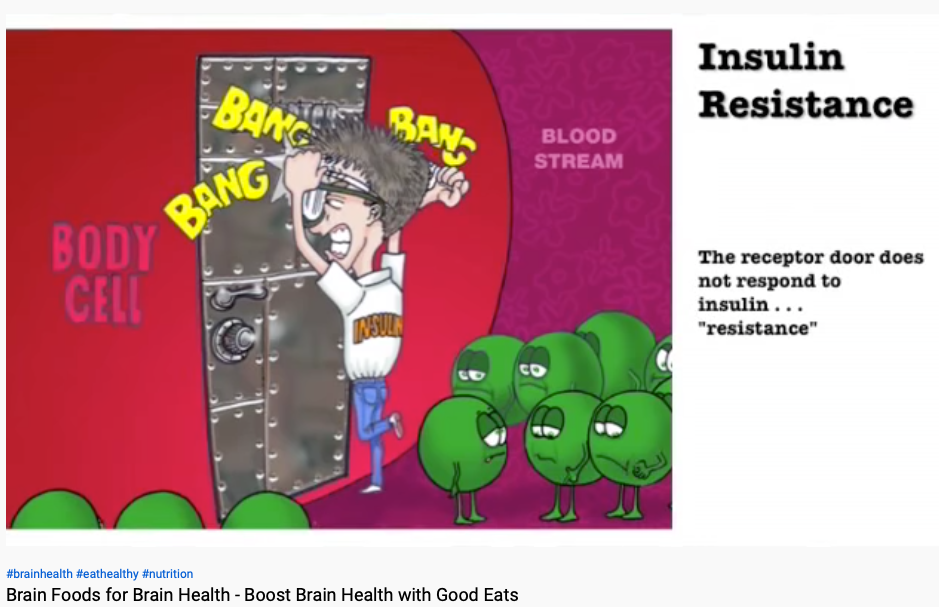
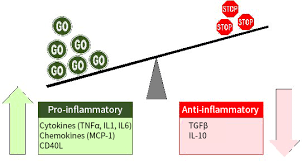 MS is also characterized by increased background levels of inflammatory cytokines. Such increases of inflammatory messengers can emanate from high levels of fatty tissue and hyperinsulinemia.2(361-362) In particular, higher levels of IL-6 and TNF-alpha have been recorded among those with obesity and hyperinsulinemia.2(361) The presence of pre-existing inflammatory cytokines/inflammation is thought/hypothesized to complicate/enhance COVID-19 since SARS-CoV-2, itself, drives excessive oxidative stress and inflammation.2(361)
MS is also characterized by increased background levels of inflammatory cytokines. Such increases of inflammatory messengers can emanate from high levels of fatty tissue and hyperinsulinemia.2(361-362) In particular, higher levels of IL-6 and TNF-alpha have been recorded among those with obesity and hyperinsulinemia.2(361) The presence of pre-existing inflammatory cytokines/inflammation is thought/hypothesized to complicate/enhance COVID-19 since SARS-CoV-2, itself, drives excessive oxidative stress and inflammation.2(361)
A third driver of severe COVID-19 symptoms includes pathophysiological mechanisms, which increase endothelial dysfunction and coagulopathy (blood clots; a complication of COVID-19). Increased blood sugar (hyperglycemia), a condition tightly associated with insulin resistance/type 2 diabetes, can contribute endothelial dysfunction (problems with blood vessels) and blood clot formation by driving oxidation and stimulating inflammatory cytokine gene expression.5 Increased adiposity and its associated inflammatory cytokines (i.e., IL-6, and TNF-alpha) are also implicated in thrombotic events and vascular disease.2(361) Considering SARS-CoV-2 already induces thrombosis/blood clotting, pre-existence of such a pathological state may worsen, or amplify, outcomes.
Having briefly considered the characteristics of MS suggested/thought to increase COVID-19 severity and outcomes, I would like to provide articles that I have written in the past, which provide strategies to control MS. Please find said articles below:
Metabolic Syndrome, Biomarkers, and Nutritional Interventions
Metabolic Syndrome, Low-Density Lipoproteins, and Fish Oil
Metabolic Syndrome and Lifestyle Interventions
Metabolic Syndrome, Diabetes, and Low Carbohydrate Diets; Exploring the Connection
Obesity and Metabolic Syndrome: Management and Prevention
Hyperinsulinemia, Type 2 Diabetes, and Low Carbohydrate Diets
Insulin Resistance, Type 2 Diabetes, and Carbohydrate Restriction
Walking, Diabetes, and Hemoglobin A1C
Processed Foods, Cardiovascular Disease, and Sodium
In conclusion, one of the major risk factors for increased COVID-19 severity includes metabolic syndrome (MS); a constellation of factors, that when combined, increase an individual’s chances of contracting conditions such as heart disease, stroke, and diabetes. Evidence has suggested that individuals who harbour MS have significantly increased risk of unfavorable COVID-19 outcomes. However, MS is modifiable via exercise, nutrition, and lifestyle interventions. Ultimately, it is my hope that increasing awareness, and providing evidence-based strategies to manage MS, will provide a means to help others, help themselves.
References
1. Kenney WL, Wilmore JH, Costill DL. Physiology of Sport and Exercise. 5th ed. Champaign, IL: Human Kinetics; 2012.
2. Yanai H. Metabolic Syndrome and COVID-19. Cardiol Res. 2020;11(6):360-365. doi: https://doi.org/10.14740/cr1181.
3. Agyemang-Yeboah F., Eghan BAJ, Annani-Akollor ME, et al. Evaluation of metabolic syndrome and its associated risk factors in Type 2 diabetes: A descriptive cross-sectional study at the komfo anokye teaching hospital, Kumasi, Ghana.Biomed Res Int. 2019:1-9. doi:https://doi.org/10.1155/2019/4562904.
4. Ni W, Yang D, Bao J, et al. Role of angiotensin-converting enzyme 2 (ACE2) in COVID-19.Critical Care. 2020;24(1):1-10. doi: https://doi.org/10.1186/s13054-020-03120-0.
5. Funk SD, Yurdagul A, Orr AW. Hyperglycemia and endothelial dysfunction in athersclerosis: Lessons from type 1 diabetes. Int J Vasc Med. 2012;2012:1-19. doi:10.1155clot/2012/569654.
-Michael McIsaac