In several of my last posts, information was provided characterizing the virulence, infectivity, general pathophysiology of SARS-CoV-2, and the ultimate manifestation of viral infection; COVID-19. Other posts have covered interventions to support the immune system including the utility of omega-3 fatty acids, vitamin D3, quercetin, zinc, vitamin C, and emerging uses of ivermectin. In the following sections, I would like to consider and explore research concerning natural immunity, vaccine efficacy, and their relationship to SARS-CoV-2.
WHAT IS NATURAL IMMUNITY?
Natural immunity can be defined as immunity acquired from direct exposure to the pathogen responsible for manifesting the disease state.1 Conversely, vaccine-induced immunity is defined as immunity acquired from a killed/weakened form of the disease through vaccination.1 mRNA technology stimulates the body to produce spike protein by introduction of mRNA coding for the same; such a procedure, however, does not appear to strictly fall under the definition of vaccine-induced immunity outlined above.
EVIDENCE TO SUPPORT NATURAL IMMUNITY
As covered in previous posts, the most vulnerable groups likely to experience severe COVID-19 outcomes included individuals of advanced age, immunocompromised, and those with metabolic syndrome.2 As such, it would seem reasonable and logical to consider vaccination (and lifestyle/nutrition/physical activity changes where appropriate) for the aforementioned cohorts. However, research is mounting (to include preprint), which has suggested the potential utility/efficacy of natural immunity that could be applicable towards non-vulnerable groups.
COMPARING VACCINE IMMUNITY AND NATURAL IMMUNITY
A prospective observational analysis, focused upon 4 cohorts: unvaccinated/recovered subjects, vaccinated subjects followed from a week after the second dose onwards, vaccinated subjects followed from one week of the first dose, and unvaccinated subjects.5 Outcome measures included breakthrough infection, hospitalization from COVID-19, severe illness, and death.5(1) Said study was a 3-month long, nationwide, and large-scale enabling an optimized assessment of vaccine and natural immunity effectiveness against the aforementioned measured outcomes.5(10) Vaccination (Pfizer) was deemed to be 92.8% protective against infection, 94.4% protective against severe illness, 94.2% effective against hospitalization, and 93.7% against death.5(1) Interestingly, prior SARS-CoV-2 infection provided 94.8% protective against infection, 96.4% effective against severe illness, and 94.1% effective against hospitalization; death was not calculated as only one death occurred in the unvaccinated/recovered cohort.5(1,10)
BREAKTHROUGH INFECTIONS
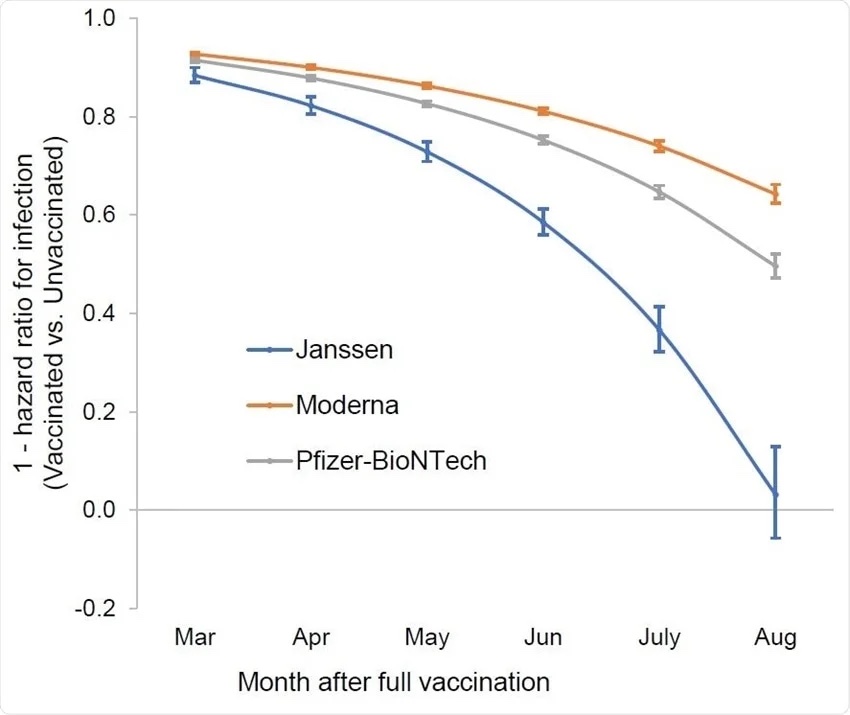
Long-term effectiveness of vaccines for viral strains (i.e., delta variant) beyond the original wild-type SARS-CoV-2, for which the mRNA vaccine was engineered for, is not completely known, though reports of waning immunity continue to emerge.3 One such study (retrospective observational study) compared 3 groups to include previously infected + single dose vaccinated individuals (42,099 subjects), previously infected individuals (62,883 subjects) who have not been vaccinated, and non-infected individuals (673,676 subjects) who received a two-dose regimen of the BioNTech/Pfizer mRNA BNT162b2 vaccine.3(2) Non-infected individuals with a two dose regimen were found to have a 13.06-fold increased risk of breakthrough infection (with the delta variant) compared to previously infected.3(2) Such indicates that immunity of the unvaccinated is likely providing a better “barrier” against new variants. As such, the researchers suggested that natural immunity conferred longer lasting and stronger protection, not only against infection, but also against symptomatic disease and hospitalization.3(3)
ANTIBODY LEVELS OVER TIME
Another preprint study by Israel et al.4 recruited a total of 7014 participants; 2653 subjects were fully vaccinated (2 doses of Pfizer) while 4361 subjects were naturally infected and recovered from SARS-CoV-2. Antibody titers (concentrations) were measured within each subject of both groups between Jan 31/2021 and July 31/2021. Higher antibody titers were observed in vaccinated individuals (median 1581 AU/ml) after the second vaccination compared to convalescent (recovered from disease) subjects (median 355 AU/ml).4(3) However, each following month, antibody titers decreased by 40% in the vaccinated group while the convalescent subjects experienced only a 5% decrement in antibody titers per month.4(3) Within 6 months, 16.1% vaccinated subjects had antibody readings below the seropositivity threshold (a method of measuring the presence of antibodies; a low threshold means the antibody concentrations are not high enough to provide immunity), while convalescent subjects only had 10.8% of their population below said threshold.4(9)
COMPARING STUDIES
The first research study of Goldberg et al.5 suggested similar effectiveness to naturally immune individuals, while the second and third studies by Gazit et al.3 and Israel et al.4, respectively, indicated larger disparities between vaccinated and unvaccinated individuals. Such might be explained by the research timeframes of Goldberg et al.5(8); subjects were largely tracked in December 20/2020 and March 20/2021, when vaccines were initially offered to the public and before the delta variant dominated in Israel. Furthermore, the observation period was only 3 months.5(6) Conversely, Israel et al.4(3) were conducting research over 6 months from January 31/2021 to July 31/2021, while the follow-up period of Gazit et al.3(2) occurred between June 1/2021 and August 14/2021.
Unlike Goldberg et al, Israel et al. implemented a time frame twice as long, which allowed periods long enough to observe waning immunity. In the case of Gazit et al, studies were taking place when the delta variant was dominating, which may have explained the high rate of breakthrough infection observed in vaccinated individuals. Since mRNA vaccine technology was designed for the original virus, it is unlikely to be effective at completely neutralizing variants; 67% effective according to Bernal et al.,6 meaning breakthrough infections, and transmission, are likely. Other research has also corroborated that vaccines have been 9-14 times less sensitive/did not show protection in neutralizing variants such as B.1.351.9,10
ADDITIONAL RESEARCH STUDIES
The aforementioned studies were presented to encourage review of emerging evidence regarding natural immunity and the strengths/weaknesses of vaccines. Said studies are a small sample of a larger set of research projects that have already occurred. Please see the web link to The Pulse below, which provides 130 studies with individual links and accompanying summaries exploring vaccine efficacy and natural immunity.
The Pulse: 130 Research Studies Affirming The Power of Natural COVID Immunity
CONCLUSIONS
Several studies provided above are in preprint (studies released in lieu of peer review), and should thus be viewed with caution. However, the large volume of research (i.e., 130 studies) conducted during the pandemic remains compelling and worthy of review, consideration, and deeper research. Finally, the survival rate of most individuals under 80 years of age exceeds 99%; a statistic that should help provide perspective and reduce fear, as one navigates through the evidence.7,8
References
1. Immunity types. Centers for Disease Control and Prevention website. Accessed November 26, 2021. https://www.cdc.gov/vaccines/vac-gen/immunity-types.htm.
2. COVID-19: Who’s at higher risk of serious symptoms? Mayo Clinic website. Updated October 30, 2021. Accessed October 31, 2021. https://www.mayoclinic.org/diseases-conditions/coronavirus/in-depth/coronavirus-who-is-at-risk/art-20483301
3. Gazit S, Shlezinger R, Perez G, Lotan R, et al. Comparing SARS-CoV-2 natural immunity to vaccine-induced immunity/l Reinfections versus breakthrough infections. MedRxiv. 2021:1-32. doi:https://doi.org/10.1101/2021.08.24.21262415.
4. Israel A, Shenhar Y, Green I, et al. Large-scale study of antibody titer decay following BNT162b2 mRNA vaccine or SARS-CoV-2 Infection. MedRxiv. 2021:1-27. doi: https://doi.org/10.1101/2021.08.19.21262111.
5. Goldberg Y, Mandel M, Woodbridge Y, et al. Protecting of previous SARS-CoV-2 infection is similar to that of BNT162b2 vaccine protection: A three-month nationwide experience from Israel. MedRxiv. 2021:1-49. doi:https://doi.org/10.1101/2021.04.20.21255670.
6. Bernal JL, Andrews N, Glower C, et al. Effectiveness of Covid-19 vaccines against the B.1.617.2 (Delta) variant.NEMJ. 2021;385(7):585-594. doi:10.1056/NEJMoa2108891.
7. Mahase E. Covid-19: Death rate is 0.66% and increases with age, study estimates. BMJ. 2020;269. doi:10.1136/bmj.m1327.
8. Meyerowitz G, Merone L. A systematic review and meta-analysis of published research data on COVID-19 infection fatality rates. Int J Infect Dis. 2020;101:138-148. doi: 10.1016/j.ijid.2020.09.1464.
9. Shen X, Tang H, Pajon R, et al. Neutralization of SARS-CoV-2 variants B.1.429 and B.1.351. N Engl Med. 2021;384(24):2352-2354. doi:10.1056/NEJMc2103740.
10. Madhi SA, Baillie V, Cutland M, et al. Efficacy of the ChadOx1 nCoV-19 Covid-19 vaccine against the B.1.351 variant. N Engl Med. 2021;384(20):1885-1898. doi: 10.1056/NEJMoa2102214.
-Michael McIsaac